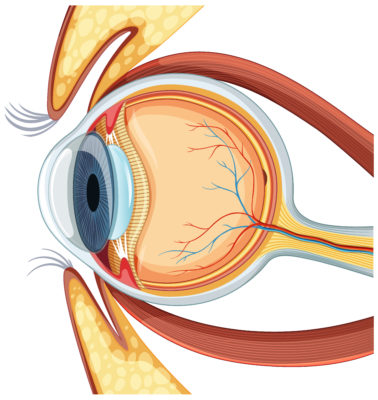
The pachymetry test is a crucial diagnostic tool used by ophthalmologists to measure the thickness of the cornea, the transparent front layer of the eye. This measurement plays a vital role in interpreting eye pressure readings and evaluating the risk of conditions such as glaucoma and keratoconus.
By accurately assessing corneal thickness, the test helps ensure that eye pressure (intraocular pressure, or IOP) readings are interpreted correctly, supporting early detection and management of eye diseases.
What is a Pachymetry Test?
The pachymetry test is a simple, non-invasive procedure that measures the thickness of the cornea in micrometres. In clinical practice, it’s often performed as part of a glaucoma evaluation or before procedures like LASIK.
So, what is the pachymetry test used for? It provides valuable insights into the thickness of your cornea, which helps doctors determine whether your eye pressure readings are accurate.
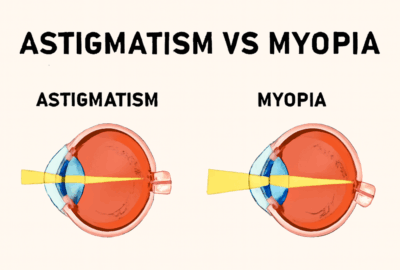
For example, if the cornea is unusually thick, the measured pressure may appear higher than it truly is. Conversely, thin corneas may show deceptively low readings.
Why Corneal Thickness Matters
Understanding the pachymetry normal range is essential for accurate eye diagnosis. The normal corneal thickness typically ranges between 520 and 540 micrometres. Deviations from this range can influence both vision quality and disease risk.
A thinner cornea may indicate higher susceptibility to glaucoma, as the eye may be more prone to pressure-related damage. On the other hand, a thicker cornea can affect intraocular pressure readings, potentially leading to overestimation.
Corneal thickness is also a critical factor before undergoing refractive surgeries like LASIK or PRK. Surgeons use pachymetry results to ensure there’s enough corneal tissue remaining after reshaping to maintain eye safety and structural integrity.
How is the Pachymetry Test Performed?
The pachymetry procedure is quick and painless. It can be performed using several different technologies, each with its own strengths depending on the patient’s eye condition. The pachymetry uses include evaluating glaucoma risk, preparing for refractive surgery, and diagnosing corneal diseases.
Before the test, your eyes may be numbed with anaesthetic drops (for contact methods). The ophthalmologist or technician then uses specialised equipment to precisely measure corneal thickness.
Optical Pachymetry
Optical pachymetry uses light waves to measure corneal thickness without physically touching the eye. It’s a non-invasive, safe, and fast method.
The device directs a light beam onto the cornea and, by analysing the reflected light, calculates the exact thickness. This method is often preferred for its comfort and high accuracy.
Optical Coherence Tomography (OCT)
OCT pachymetry uses advanced light reflection technology to generate detailed cross-sectional images of the cornea. It captures the layers of the cornea in high resolution, allowing doctors to assess both thickness and structural integrity. OCT is particularly useful in patients with corneal diseases or irregularities, providing data beyond simple thickness measurements.
Scheimpflug Imaging
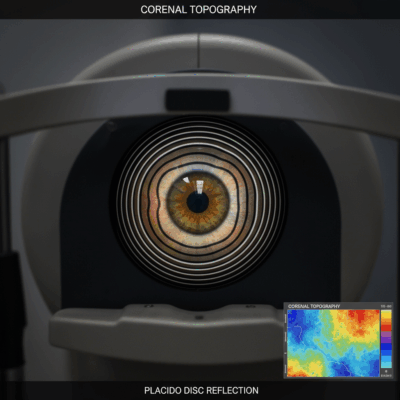
Scheimpflug imaging employs a rotating camera combined with optical analysis software to capture detailed 3D images of the cornea and anterior eye segment. It provides precise pachymetry readings, even in eyes with irregular corneas or scarring. This method is especially useful for patients planning refractive surgery or those diagnosed with keratoconus.
Uses and Benefits of Pachymetry
Pachymetry uses extend across various aspects of ophthalmology. It is not only diagnostic but also helps guide treatment planning and monitor long-term eye health.
- Glaucoma Screening: Determines accurate intraocular pressure readings and assesses the risk of optic nerve damage.
- Refractive Surgery Planning: Ensures adequate corneal thickness before procedures such as LASIK or SMILE.
- Monitoring Corneal Diseases: Helps track conditions such as keratoconus, corneal oedema, or dystrophies.
- Post-Surgery Evaluation: Monitors corneal healing after refractive or transplant procedures.
Who Should Get a Pachymetry Test?
A pachymetry test is often recommended for patients at higher risk of glaucoma or those planning vision correction surgeries. It is also advised for:
- Individuals with a family history of glaucoma.
- People diagnosed with thin or irregular corneas.
- Patients who have undergone previous eye surgeries.
- Those experiencing unexplained fluctuations in intraocular pressure.
Advancements in Pachymetry Technology
Modern pachymetry devices have evolved to provide higher accuracy and faster results. Earlier ultrasound-based models required direct contact, but newer optical systems such as OCT and Scheimpflug imaging have improved comfort and precision.
Today’s machines can capture thousands of data points across the cornea in seconds, offering complete topographic maps. These advancements not only enhance diagnostic reliability but also improve patient experience during testing.
When Should You See a Doctor for a Pachymetry Test
If you are at risk of glaucoma, have a family history of eye diseases, or are considering refractive surgery, a pachymetry test is strongly recommended. It provides vital data about your corneal structure, helping doctors tailor treatments accordingly.
Regular eye examinations that include pachymetry can detect subtle corneal changes before they cause vision problems. Discuss the test with your ophthalmologist if you notice blurred vision, frequent prescription changes, or conditions such as diabetes or high myopia, which increase the risk of eye disease.