Introduction – Why Understanding Eye Pressure Matters
Intraocular pressure (IOP) refers to the fluid pressure inside the eye, measured in millimetres of mercury (mm Hg). It helps maintain the eye’s shape and ensures the cornea and optic nerve receive essential nourishment.
When IOP rises too high or falls too low, it can damage the optic nerve and lead to vision problems or permanent sight loss. Understanding the eye pressure range, monitoring fluctuations, and recognising risks are essential for protecting long-term vision. Many people only discover abnormal pressure during routine check-ups, which reinforces why regular monitoring is important.

What Is a Normal Eye Pressure Range?
Typical Eye Pressure Levels
A normal eye pressure range usually falls between 10 and 20 mm Hg, although some clinicians consider 10-21 mm Hg acceptable. Pressures above 21 mm Hg may indicate ocular hypertension, while levels below 10 mm Hg suggest ocular hypotony.
Importantly, some individuals develop optic nerve damage even within the normal eye pressure range, indicating that this range is a guideline rather than a guarantee of safety. Factors such as corneal thickness, family history, and optic nerve structure influence individual susceptibility.
Why Eye Pressure Varies
IOP is not static. It fluctuates throughout the day due to fluid production and drainage, body position, time of day, and medication use. Morning readings are often higher. These patterns of eye pressure variation help doctors evaluate risk, as large fluctuations may be as concerning as consistently elevated pressure.
Causes of High and Low Eye Pressure
What Causes High Intraocular Pressure?
High IOP results from an imbalance between fluid inflow and outflow. If aqueous humour drains poorly or is produced excessively, pressure rises. Risk factors include eye trauma, uveitis, steroid use, age over 40, pigment dispersion syndrome, family history of glaucoma, diabetes, hypertension and thyroid disorders.
High pressure usually has no symptoms until significant optic nerve damage occurs, making early detection crucial. These causes of high eye pressure often contribute to the development of glaucoma.
What Causes Low Eye Pressure?
Low IOP, or ocular hypotony, may develop after eye surgery, injury, severe inflammation or reduced fluid production. Sudden drops can distort ocular structures, leading to blurred vision, headaches, or retinal complications. Understanding the causes of ocular hypotony helps patients recognise when urgent care is needed.
Risk Factors & Related Eye Conditions
Who Is at Risk for Abnormal Eye Pressure?
People over 40, those with a family history of glaucoma, individuals of African American, Hispanic or Asian descent and those with diabetes, high blood pressure or myopia face increased risk. Lifestyle factors such as smoking, high caffeine intake, inadequate sleep and tight collars may also influence pressure. These eye pressure risk factors highlight why regular screening is important.
Eye Conditions Linked to Pressure Problems
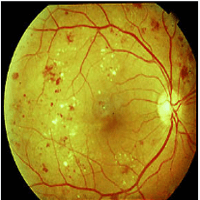
Ocular hypertension refers to elevated pressure without optic nerve damage, but it increases glaucoma risk. Glaucoma occurs when high pressure damages the optic nerve, causing gradual vision loss.
Normal tension glaucoma develops at normal pressures, demonstrating that optic nerve vulnerability varies. Low pressure can cause hypotony-related changes such as retinal folds. Understanding ocular hypertension vs glaucoma supports early intervention.
Signs & Symptoms Indicating You Should Check Your Eye Pressure
Most people with abnormal IOP experience no symptoms until the late stages. Warning signs include blurred or tunnel vision, halos around lights, pain or pressure in the eye, headaches, redness or sudden loss of side vision.
Immediate evaluation is essential if symptoms appear suddenly, as they may indicate acute angle closure glaucoma. Recognising symptoms of high eye pressure ensures timely care.
How Eye Pressure Is Measured
Tonometry Methods
IOP is measured using tonometry. Goldmann applanation tonometry is the gold standard: after applying numbing drops, a device gently flattens the cornea to calculate pressure.
Non-contact tonometry uses a puff of air and requires no drops. Handheld devices such as Tono-Pen or rebound tonometers help assess pressure in children or in emergency settings. All eye pressure test methods are quick and painless.
What to Expect During an Eye Pressure Test
Patients rest their chin and forehead on a support while the device touches the cornea or releases a small puff of air. The test lasts seconds, and multiple readings may be taken to account for fluctuations.
Frequency of Eye Exams & Pressure Monitoring
Adults aged 40-54 should have comprehensive exams every 2-4 years, those 55-64 every 1-3 years and individuals aged 65+ every 1-2 years. Patients with risk factors, such as diabetes or hypertension, may need annual exams. This pressure monitoring schedule supports early detection.
Monitoring & Managing Eye Pressure at Home
Some glaucoma patients use home tonometry devices to track pressure trends. Lifestyle habits that support stable IOP include drinking fluids gradually, avoiding inverted postures, wearing protective eyewear, and limiting caffeine intake.
Maintaining a healthy weight, exercising regularly and managing systemic diseases like diabetes and hypertension also help. Patients should use prescribed drops correctly and attend follow-up visits. These strategies support monitoring eye pressure at home.
Treatment Options for High & Low Eye Pressure
Medications for Elevated Eye Pressure
Eye drops include prostaglandin analogues, beta blockers, alpha-agonists, carbonic anhydrase inhibitors, nitric oxide donors, and rho kinase inhibitors. Oral carbonic anhydrase inhibitors may be used for short-term emergencies. Treatment choice depends on pressure levels and optic nerve health.
Laser & Surgical Treatments
Selective laser trabeculoplasty (SLT) improves fluid drainage. Surgical options such as trabeculectomy or tube shunt procedures create new drainage pathways for advanced glaucoma. These laser eye pressure treatment approaches help protect vision when drops are insufficient.
Managing Low Eye Pressure
Treating hypotony involves addressing the underlying cause, such as repairing a wound leak or reducing inflammation. Steroids or NSAIDs may restore stability. Sudden low pressure requires prompt specialist care.
Preventing Eye Pressure Problems & Supporting Eye Health
Lifestyle measures include a balanced diet, regular exercise, weight control, limiting caffeine intake, quitting smoking, and getting adequate sleep. Managing systemic conditions supports optic nerve health. Wearing protective eyewear prevents injury. Regular exams ensure early detection of abnormalities.
Conclusion: Protect Your Vision by Monitoring Eye Pressure
Maintaining your vision starts with understanding and monitoring your IOP. While a normal eye pressure range is generally 10-20 mm Hg, the critical factors are your individual eye health and the resilience of your optic nerve.
Both elevated and abnormally low pressure pose a serious risk of irreversible vision loss if left unaddressed. By adhering to a schedule of routine eye exams, adopting healthy lifestyle choices, and diligently following your ophthalmologist’s guidance, you take the most proactive steps toward securing your long-term eye health and protecting your sight.