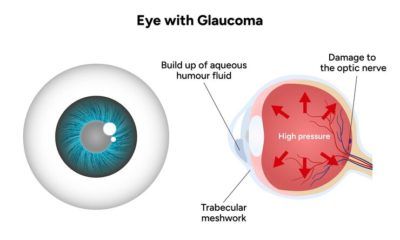
Glaucoma is a leading cause of irreversible vision loss, often linked to raised intraocular pressure (IOP). One of the most effective ways to treat certain types of glaucoma, especially angle-closure glaucoma, is laser iridotomy.
This minimally invasive procedure utilises focused laser energy to create a small opening in the iris, thereby improving fluid drainage and reducing pressure within the eye. It plays a vital role in preventing optic nerve damage and preserving vision.
What is Laser Iridotomy?
Laser iridotomy is a quick outpatient procedure designed to improve fluid outflow in patients with narrow or closed drainage angles.
By creating a small hole in the iris, the fluid (aqueous humour) flows more freely, preventing sudden rises in pressure. This technique is primarily used in angle-closure glaucoma but is sometimes recommended for patients at risk of developing the condition.
Laser Iridotomy vs. Other Glaucoma Treatments
Unlike eye drops or oral medications that focus on lowering pressure chemically, laser iridotomy addresses the structural cause of blocked drainage.
While trabeculectomy and glaucoma drainage implants are surgical approaches, iridotomy is less invasive, quicker, and has fewer complications. It is often the first-line choice in preventing acute angle-closure episodes, which can be a medical emergency.
Benefits of Laser Iridotomy
Prevents Complications Like Angle Closure.
One of the primary benefits of laser iridotomy is the prevention of acute angle-closure glaucoma. By creating a bypass route in the iris, the risk of sudden, painful pressure spikes is significantly reduced.
Improves Drainage and Intraocular Pressure Control
The procedure helps restore balance by improving the flow of aqueous humour. This leads to better control of intraocular pressure, reducing the long-term risk of optic nerve damage and subsequent vision loss.
Types of Laser Iridotomy
YAG Laser Iridotomy
The YAG laser is the most commonly used technique. It delivers short, precise bursts of energy to the iris, creating a clean, controlled opening. It is effective, quick, and widely available in ophthalmology clinics.
Laser Peripheral Iridotomy
The laser peripheral iridotomy technique involves creating a hole in the outer part of the iris. It is strategically placed under the upper eyelid to minimise light scatter or visual disturbances. It helps maintain normal eye function while improving fluid drainage.
Comparison of Techniques
Both YAG and peripheral iridotomy are safe and effective. The main difference lies in the laser type and placement of the opening. YAG is versatile and commonly preferred, while peripheral placement reduces visual symptoms like glare or halos.
When Is Laser Iridotomy Necessary?
Indications for Procedure
Laser iridotomy is recommended when patients show signs of narrow or closed angles on eye examination. It may also be advised in cases where patients are at high risk of an acute attack.
Conditions Treated by Laser Iridotomy
It is primarily used for primary angle-closure glaucoma but may also help in secondary forms of glaucoma caused by trauma, lens changes, or other structural abnormalities blocking fluid outflow.
Primary Angle-Closure Glaucoma
This condition arises when the iris blocks the drainage angle, trapping fluid inside the eye. Laser iridotomy creates an alternative route, preventing sudden vision-threatening increases in eye pressure.
Secondary Glaucoma
In cases where trauma, inflammation, or other eye diseases lead to secondary angle-closure, laser iridotomy can relieve blockages and improve fluid balance. It may be combined with other treatments for better outcomes.
How Is Laser Iridotomy Performed?
The procedure is usually performed under topical anaesthetic drops. A contact lens is placed on the eye to focus the laser.
The ophthalmologist then applies pulses of light to create a small iris opening. The procedure usually takes only a few minutes, and most patients return home the same day.
What Are the Risks and Side Effects of Laser Iridotomy?
Mild Eye Discomfort
Some patients may feel a temporary stinging sensation or mild discomfort during or after the procedure. This usually subsides quickly with prescribed anti-inflammatory drops.
Temporary Blurred Vision
Mild blurriness may occur for a few hours after treatment due to pupil changes and light scatter. Vision usually stabilises by the following day.
Increased Sensitivity to Light
Patients may notice slight glare or light sensitivity for a short period after laser iridotomy. Using sunglasses can help reduce discomfort until the eyes adjust.
Minor Inflammation and Irritation
The laser may cause mild inflammation inside the eye. This is usually controlled with topical steroids or anti-inflammatory eye drops prescribed after the procedure.
How is the Recovery and Aftercare for Laser Iridotomy?
Recovery Timeline
The laser iridotomy recovery time for most patients is within 24-48 hours. Normal activities can often be resumed within a day, although some temporary vision fluctuations may occur during the initial recovery phase.
Post-Procedure Care Tips
Doctors usually prescribe anti-inflammatory drops to reduce irritation. Patients should avoid rubbing their eyes and follow medical advice about activity levels. Protective sunglasses can help reduce sensitivity to light.
Monitoring After Surgery
Follow-up visits are essential to ensure that the opening remains functional and that intraocular pressure is controlled. Regular eye pressure checks help in detecting any complications early.
What is the Success Rate of Laser Iridotomy?
Laser iridotomy has a high success rate in preventing angle-closure attacks, with success rates exceeding 90%. However, patients may still require additional glaucoma treatments, such as drops or surgery, to maintain long-term pressure control.
Conclusion
Laser iridotomy is a proven and highly effective treatment for managing certain types of glaucoma, particularly angle-closure glaucoma. Creating a small passage in the iris improves fluid drainage and prevents dangerous rises in intraocular pressure.
While generally safe and quick, it requires follow-up care to monitor effectiveness. Patients at risk of angle-closure should discuss the procedure with their ophthalmologist to understand its benefits, risks, and alternatives for preserving healthy vision.