A mature cataract is an advanced stage of cataract in which the eye’s natural lens becomes completely opaque, leading to significant vision loss. At this stage, daily tasks like reading, driving, or recognising faces become extremely difficult.
Cataract progression varies among individuals, but if untreated, a mature cataract may cause severe complications. This guide explains the causes, symptoms, stages, and available treatments, while comparing the differences between mature and immature cataracts.
What Is a Mature Cataract?
Understanding Cataract Development
Cataracts form when proteins in the lens clump together, preventing light from passing through clearly. This process, known as cataract development, results in blurred or cloudy vision.
Over time, cataracts progress from an early immature stage to a fully opaque lens, known as a mature cataract, where vision is severely compromised. Understanding how cataracts progress is crucial for timely intervention and prevention of permanent visual impairment.
How Does a Cataract Mature?
A cataract becomes mature when the lens is completely clouded, leaving patients able to perceive only light and dark without clear detail. This cataract maturation process represents the final stage of opacity.
The mature cataract’s meaning is complete opacification, where corrective lenses no longer improve vision. Unlike immature cataracts that only partially obscure the lens, mature cataracts completely block light entry into the eye.
Causes of Mature Cataracts
Ageing and Lens Protein Breakdown
The leading cause of mature cataract is natural ageing. With time, proteins in the lens break down and clump together, making the lens hard and opaque. This age-related degeneration is the most common risk factor for mature cataracts, especially in adults over 60 years old.
Diabetes and Metabolic Factors
Poorly controlled diabetes accelerates cataract progression. Elevated blood sugar levels affect lens metabolism, leading to faster protein clumping and lens clouding. Among the causes of mature cataract, diabetes remains a critical metabolic factor, especially when left untreated for long periods.
UV Exposure and Lifestyle Habits
Prolonged exposure to ultraviolet (UV) radiation can damage lens proteins, speeding cataract development. Lifestyle habits such as smoking and excessive alcohol consumption are also key risk factors for mature cataract. These factors accelerate clouding and bring cataracts to the mature stage earlier than expected.
Injuries, Steroids and Genetics
Eye injuries, prolonged steroid use, and genetic predisposition all contribute to the development of cataracts. In some individuals, inherited conditions increase the likelihood of reaching the mature stage earlier. Family history plays a significant role in predicting the causes of mature cataract.
Symptoms and Signs to Watch For
Vision Changes and Loss
Patients with a mature cataract experience severe vision impairment. They may struggle to recognise faces, read, or see clearly in bright light. Unlike earlier stages, mature cataracts cause almost complete blindness, making urgent medical attention necessary.
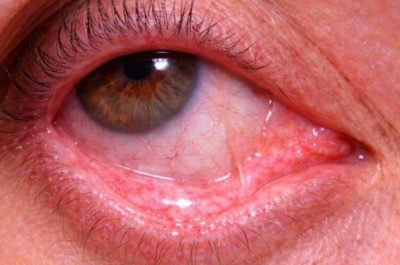
Visible Changes in the Eye
One hallmark of mature cataracts is visible eye changes. The lens appears milky, brownish, or greyish, and the pupil often looks white. Patients report faded or yellowed colours, with no iris shadow visible during examination.
Mature vs Immature Cataract Symptoms
In the mature vs immature cataract symptoms comparison, immature cataracts show mild cloudiness with some preserved vision. In contrast, mature cataracts present with complete lens opacity and severe vision loss.
The distinction between mature and immature cataracts helps doctors determine the urgency of treatment.
Types and Stages of Mature Cataracts
Nuclear Cataracts
A nuclear mature cataract develops in the central part of the lens. Initially, it causes yellowing and can temporarily improve near vision. As it progresses, the lens hardens, turns brown, and significantly reduces contrast sensitivity.
Cortical Cataracts
A cortical mature cataract starts at the outer edges of the lens, forming spoke-like opacities. These opacities scatter light, increasing glare sensitivity, especially at night while driving. Cortical cataracts eventually progress inward, causing complete lens opacity.
Brunescent and Milky Cataracts
Brunescent cataracts are dark brown, while milky cataracts appear whitish or grey. Both represent advanced types of mature cataract that complicate surgery. Recognising these subtypes ensures ophthalmologists choose the correct surgical approach for effective removal.
Diagnosing a Mature Cataract
Eye Examinations and Tests
Diagnosing mature cataract requires comprehensive eye testing. Ophthalmologists perform visual acuity tests, slit-lamp examinations, and sometimes an ultrasound to evaluate dense cataracts. These eye tests for mature cataract confirm severity and determine if surgery is urgently needed.
Why Early Diagnosis Matters
Early diagnosis helps detect cataracts before they mature and progress. Regular eye exams allow ophthalmologists to intervene at the right stage, preventing complications such as lens-induced glaucoma. Without timely intervention, the risk of mature cataract complications increases significantly.
Treatment Options for Mature Cataract
Why Surgery Is the Only Effective Treatment
Unlike early cataracts managed with glasses or lifestyle changes, a mature cataract treatment requires surgery. No medication or eye drops can reverse advanced opacification. Surgery restores clear vision by removing the opaque lens and replacing it with an intraocular lens.
Phacoemulsification: The Modern Standard
Phacoemulsification for mature cataract is the most common surgical approach. It uses ultrasound energy to break the hardened lens into fragments, which are then suctioned out through a small incision. This minimally invasive technique allows faster healing.
Extracapsular Cataract Extraction (ECCE)
In cases where the cataract is extremely dense, extracapsular cataract extraction is performed. ECCE involves removing the lens in one piece through a larger incision. While less common today, it remains a key technique for advanced cases.
Choosing an Intraocular Lens (IOL)
During surgery, the cloudy lens is replaced with an artificial intraocular lens. Options include monofocal, multifocal, and toric lenses. Selecting the right IOL options for mature cataract surgery depends on the patient’s lifestyle and visual requirements.
Risks of Delaying Treatment
Delaying treatment may cause severe mature cataract complications such as blindness, lens-induced glaucoma, and intraocular inflammation. These risks highlight why timely surgery is essential for restoring vision and preventing permanent damage.
Recovery, Aftercare and Prevention
Post-Surgery Care and Healing
Recovery after mature cataract surgery involves using prescribed eye drops, protecting the eye with shields, and avoiding strenuous activity. Regular follow-ups ensure proper healing and help detect any early signs of complications.
Lifestyle Tips to Slow Cataract Progression
Although surgery is the only effective treatment for mature cataracts, lifestyle choices can help slow progression. Wearing UV-protective sunglasses, managing diabetes, consuming antioxidant-rich foods, and quitting smoking all support eye health and delay cataract development.
Early Detection and Regular Eye Exams
Routine eye check-ups allow doctors to identify mature and immature cataracts at early stages. Detecting cataracts before they mature prevents complications and ensures timely treatment, reducing the likelihood of advanced vision loss.
Conclusion
A mature cataract severely impairs vision, but modern surgical options provide excellent outcomes. Understanding the difference between mature and immature cataract, recognising symptoms, and seeking timely treatment are crucial. With proper diagnosis, advanced surgical care, and preventive measures, patients can protect their sight and maintain independence.