Symblepharon is an eye condition that develops when abnormal adhesions form between the inner surface of the eyelid and the surface of the eyeball. These adhesions usually result from severe inflammation, injury, or scarring of the conjunctiva.
While mild cases may cause minimal discomfort, advanced symblepharon can restrict eye movement, interfere with vision, and significantly affect eye comfort. Early diagnosis and appropriate management are essential to prevent long-term complications.
What Is Symblepharon? Understanding the Condition
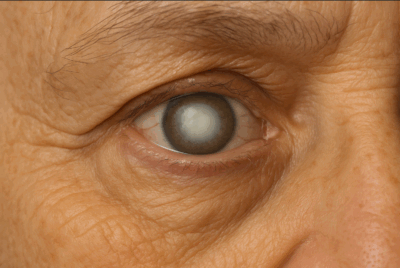
Symblepharon refers to a pathological adhesion between the bulbar conjunctiva covering the sclera and the palpebral conjunctiva lining the eyelid. In simple terms, the eyelid becomes partially or completely stuck to the eyeball. This explains the commonly used meaning of symblepharon in clinical practice.
Symblepharon is most often an acquired condition, developing after significant conjunctival inflammation or trauma rather than being present at birth. The condition primarily affects the symblepharon eye surface and can vary widely in severity.
How Symblepharon Develops
Severe inflammation causes conjunctival tissues to swell and lose their normal smooth surfaces. When opposing inflamed surfaces come into contact, healing may occur through scarring rather than regeneration.
Over time, this scarring leads to fibrous adhesions. Recurrent inflammation increases the likelihood of persistent or worsening adhesions.
Why Does Symblepharon Happen? Causes and Risk Factors
Understanding the causes of symblepharon is critical for both prevention and management. The condition arises when the conjunctiva undergoes scarring due to external or internal insults.
External Causes: Burns, Infections and Surgery
Chemical burns, especially alkali injuries, are among the most severe causes. Thermal burns, penetrating eye injuries, chronic infections, pterygium, and complications following eye surgery can all lead to extensive conjunctival inflammation and adhesion formation. Inappropriate use of certain topical medications may also contribute.
Internal Causes: Autoimmune and Systemic Diseases
Autoimmune disorders are major contributors. Conditions such as Stevens-Johnson syndrome, ocular cicatricial pemphigoid, mucous membrane pemphigoid, lichen planus, sarcoidosis, and granulomatosis with polyangiitis cause chronic conjunctival inflammation that predisposes patients to symblepharon.
Other Risk Factors: Trauma, Chronic Inflammation, Medications
Repeated episodes of conjunctivitis, ocular trauma, adverse drug reactions, and systemic conditions like graft-versus-host disease increase risk. Chronic dry eye can worsen inflammation and promote scarring when left untreated.
Variants and Types of Symblepharon
Several symblepharon types are recognised based on location and severity:
- Anterior symblepharon, where the eyelid margin adheres to the globe
- Posterior symblepharon, involving the conjunctival fornix
- Total symblepharon, with complete fusion of eyelid and eyeball
Other classifications include simple versus cicatricial forms and rare congenital variants.
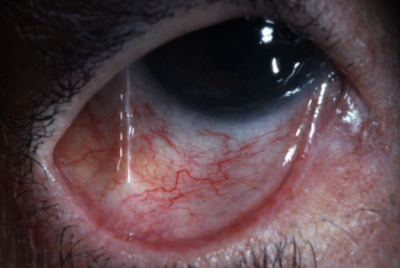
Recognising the Symptoms: How Symblepharon Affects the Eye
Symblepharon symptoms range from mild irritation to severe visual impairment. Clinically, a visible band of tissue connecting the eyelid to the eyeball is often apparent.
Visual Signs and Mechanical Issues
Adhesions may cause ptosis, entropion, or lagophthalmos. Restricted eyelid movement can prevent complete blinking, increasing exposure-related damage.
Discomfort and Irritation
Patients often experience redness, light sensitivity, excessive tearing, and persistent dryness. These symptoms worsen if the tear film is disrupted.
Movement and Functional Problems
Restricted eye movement can lead to diplopia. Adhesions may also obstruct tear drainage, resulting in chronic discomfort and recurrent infections.
Diagnosis: How Eye Specialists Detect Symblepharon
Diagnosing symblepharon involves a detailed slit-lamp examination. The clinician assesses the extent and location of adhesions and evaluates associated complications such as corneal damage. Additional tests, including conjunctival swabs or blood investigations, may be required to identify autoimmune or infectious causes.
Treatment Options: Managing and Treating Symblepharon
Effective symblepharon treatment depends on severity and underlying cause. Early intervention aims to control inflammation and prevent adhesion formation.
Medical Management to Prevent and Treat Early Symblepharon
Corticosteroids help suppress inflammation, while antibiotics or antivirals treat infections. Immunomodulators may be required for the treatment of autoimmune diseases. Lubricating eye drops reduce dryness, and amniotic membrane dressings can limit scarring once inflammation subsides.
Surgical Treatment: When Medication Isn’t Enough
Symblepharon surgery is indicated when adhesions restrict movement or threaten vision. Surgical release involves separating scar tissue and reconstructing normal anatomy. Techniques may include tissue grafts, oculoplastic reconstruction, amniotic membrane transplantation, or limbal stem cell transplantation in severe cases.
Living with Symblepharon and Aftercare
Post-treatment care focuses on lubrication, protection, and close follow-up. Prognosis varies. Some patients recover fully, while others experience recurrence or chronic symptoms.
Complications and Prognosis: What to Expect
Untreated symblepharon can lead to corneal abrasions, ulcers, chronic pain, reduced vision, and cosmetic concerns. Prognosis depends on early detection, disease control, and adherence to treatment.
Prevention Tips: How to Avoid Symblepharon
Prompt treatment of severe conjunctivitis or eye injuries is essential.
- Wear Protection: Use safety eyewear during hazardous activities to prevent chemical or thermal burns.
- Manage Systemic Health: Work with doctors to control autoimmune or inflammatory diseases that affect the eyes.
- Medication Safety: Use topical eye medications strictly as prescribed to avoid adverse tissue reactions.
Conclusion:
Symblepharon is a serious but manageable condition caused by conjunctival scarring after inflammation or trauma. Early recognition, accurate diagnosis, and timely medical or surgical care are vital to preserve comfort and vision. Addressing underlying causes remains central to long-term success.