Rajni, a 32-year-old working professional, has been working as a content writer for the past 7 years. Even though her job is hectic and tiresome, she finds satisfaction in efficiently completing all her tasks by the end of the day. One evening, when she returned from the office, she realized that she had been experiencing chronic headaches for the past couple of weeks.
She talked to her mother about her recurring headaches. Her concerned mother asked her if she had any other symptoms. While talking to her, she realized that she had vision difficulties while driving back home the other day. Assuming that she had refractive errors, she decided to get in touch with us.
When Rajni walked in, her gentle demeanour and broad smile filled the air with positivity. We asked her to take a seat, made her feel comfortable and learned more about her symptoms. After running several tests like slit-lamp examination, pachymetry, and corneal topography, we realized that Rajni might be suffering from Keratoconus.
Keratoconus: A Comprehensive Insight
In simple terms, irregularities of the cornea’s surface and thinning of the cornea are referred to as Keratoconus. The cornea is a transparent and clear outer layer of the eye. Additionally, the middle layer, which is the thickest part of the cornea, is made up of collagen and water. If a person is diagnosed with Keratoconus, the cornea begins to thin and eventually bulges into a cone shape, often resulting in loss of vision.
Once we broke the news to Rajni, she was perplexed. Most people don’t realize that they have Keratoconus symptoms are similar to those found in almost every other eye disease. After coming to terms with the reality, she inquired about the causes of Keratoconus.
This eye disease has been a subject of study for several decades, yet it remains misunderstood. After so many years of extensive research, it is interesting to note that the primary cause of Keratoconus remains unknown. However, it is believed that the predisposition to this disease is present by birth in some people.
The loss of collagen in the cornea of the patient’s eye is a common finding in keratoconus cases. Here is list of some other keratoconus symptoms to have complete clarity of this condition:
Types of Keratoconus Symptoms:
-
Eye pains and chronic headaches
-
Difficulty with night vision
-
Sensitivity to bright light
-
Clouding of vision
-
Eye irritation
-
Experiencing glare
-
Halos around lights
Risk factors for Keratoconus
Be it any disease, some people are more prone to it than others. Below is an overview of the risk factors for Keratoconus:
-
Genetics
Patients are more likely to develop Keratoconus if they have Downs syndrome or certain systemic diseases in their family history.
-
Chronic Irritation in Eyes
Allergies or other irritants can cause chronic inflammation, which can lead to corneal tissue loss and the development of Keratoconus.
-
Age
Teenagers are frequently the first to learn they have Keratoconus. Younger patients with severe Keratoconus are typically more likely to require surgical intervention as the condition worsens.
-
Chronic Eye Rubbing
Keratoconus development is also linked to persistent eye rubbing. If not, it might increase the likelihood of the disease getting worse.
A Glimpse into Keratoconus Treatment
Keratoconus treatment focuses on vision correction, which directly depends on the stage of the disease. Basically, keratoconus treatment can be divided into three parts or divisions: early stage, intermediate stage and advanced stages.
-
Early Stages
Currently, keratoconus treatment in the early stages includes glasses to treat astigmatism and near-sightedness. However, as Keratoconus worsens, these glasses turn redundant in providing clear vision. Such patients will have to wear hard contact lenses.
-
Intermediate Stages
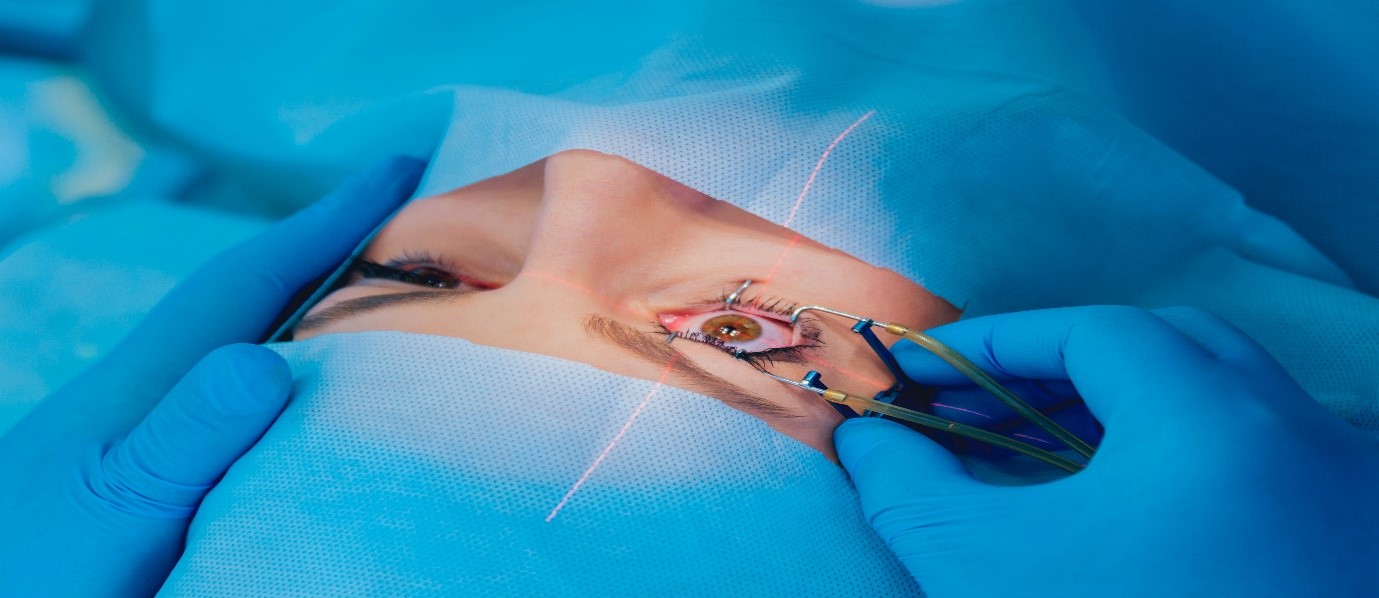
This stage is also called progressive Keratoconus; in most cases, it is treated with corneal collagen cross-linking. This process involves the application of the vitamin-B solution, which is further activated by UV light for 30 minutes or less. As a result, this solution generates new collagen bonds, preserving and recovering the cornea’s shape and strength.
-
Advanced Stages
-
Corneal Ring
A regular contact lens may become too unpleasant to wear if you have severe Keratoconus. Intacs are plastic, implantable C-shaped rings that flatten the cornea’s surface to enable better vision. The completion of this process takes about 15 minutes.
-
Corneal Transplant
A donor cornea replaces the patient’s injured cornea during this transplant. The procedure for a corneal transplant usually takes one hour and is done as a day care procedure. Following the transplant, vision is typically hazy for three to six months, and medication is required to prevent transplant rejection. In order to improve the patient’s vision after transplant surgery, glasses or contact lenses are required.
Fortunately, when Rajni visited us, her condition was still in the early stage. Therefore, after careful examination, we prescribed her glasses for near-sightedness.
Dr Agarwals Eye Hospital: Bringing You the Best Eyecare Since 1957
At Dr Agarwal’s Eye Hospital, from routine eye-check-ups to critical eye surgeries, we provide holistic eye treatments. In addition, we also offer a diversified range of treatments like oculoplasty, PDEK, glued IOL, cataract surgery, photorefractive keratectomy, and more.
We deliver the best eye care across the globe in 11 countries at our 110+ hospitals. Explore our official website to know more.