Understanding Dacryocystitis
Early and appropriate treatment of dacryocystitis is important because the condition can progress quickly if left unmanaged. Many patients ask what dacryocystitis is, and the answer begins with the tear drainage system. The condition refers to an infection or inflammation of the lacrimal sac.
The sac becomes infected when the nasolacrimal duct is blocked, leading to tears stagnating and allowing bacteria or viruses to multiply. Understanding tear drainage helps explain why obstructions lead to swelling, pain and discharge.

What Causes Dacryocystitis?
Several dacryocystitis causes can trigger infection. A blocked tear duct is the most common factor. In newborns, a persistent membrane at the duct opening often causes blockage. In adults, age-related narrowing, trauma, chronic sinusitis, nasal structural issues, previous surgeries, immune-related conditions or tumours can hinder tear drainage.
Certain medications such as timolol, dorzolamide, pilocarpine and trifluridine may also contribute. Congenital dacryocystitis occurs when amniotic fluid fails to drain before birth.
Recognising Dacryocystitis Symptoms
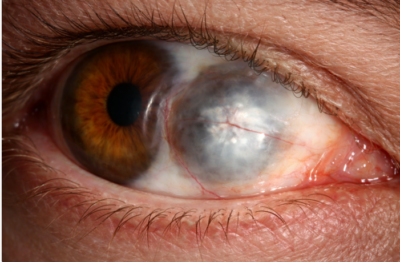
Identifying dacryocystitis symptoms early improves outcomes. Acute dacryocystitis presents with sudden pain at the inner corner of the eye, swelling, redness and fever.
Pus may accumulate and form an abscess. Chronic dacryocystitis produces milder symptoms, such as persistent tearing and intermittent discharge, without fever. Infants may show watering and sticky eyes as the main signs.
How Dacryocystitis Is Diagnosed
Accurate dacryocystitis diagnosis helps guide the correct treatment approach. Doctors begin with a history and physical examination. Gentle pressure over the sac may release discharge, confirming blockage and infection. Additional tests include:
- Culture tests to identify bacteria
- Blood tests to detect inflammation
- Fluorescein dye disappearance test to check drainage
- Imaging, such as CT or dacryocystograph, is performed when structural abnormalities are suspected
Early diagnosis ensures that dacryocystitis treatment is initiated promptly to avoid complications.
Best Ways to Treat Dacryocystitis
Effective dacryocystitis treatment combines medical therapy, supportive care and, when necessary, surgical procedures. Identifying the best ways to treat dacryocystitis depends on whether the condition is acute, chronic or congenital.
Medical Treatments – Antibiotics and Pain Relief
Acute dacryocystitis generally responds to oral or intravenous antibiotics such as amoxicillin-clavulanate, cephalexin, ciprofloxacin or clindamycin. Topical antibiotic drops or ointments may support treatment.
Pain and swelling are managed with warm compresses and analgesics. Infants with congenital dacryocystitis often improve naturally but may need antibiotics during flare-ups.
Home Remedies to Ease Discomfort
Supportive care can help relieve pain. Warm compresses applied several times a day loosen debris and reduce swelling.
Gentle massage of the lacrimal sac may help expel discharge. These dacryocystitis home remedies assist medical therapy but do not replace professional care. Good hand hygiene prevents further irritation.
Surgical Options – Dacryocystorhinostomy and Other Procedures
When medical therapy fails or obstruction persists, dacryocystitis surgery offers long-term relief. Dacryocystorhinostomy (DCR) is the standard procedure. It creates a new drainage pathway from the tear sac into the nose.
Other surgical options include probing, balloon dacryoplasty and stenting. These techniques help restore tear flow and prevent recurrences. Surgical decisions depend on age, the severity of the blockage, and the response to previous treatments.
Dacryocystitis Treatment in Children vs Adults
Dacryocystitis treatment for children differs from that for adults. Many infants improve within 6-12 months, especially with Crigler massage and topical antibiotics. Persistent symptoms may require probing or DCR after one year.
In adults, dacryocystitis treatment usually requires oral antibiotics, with chronic cases often needing DCR. Adult ducts rarely unblock spontaneously, making procedural treatment important for long-term relief.
Preventing Dacryocystitis
Several steps help prevent dacryocystitis:
- Avoid touching or rubbing the eyes with unwashed hands
- Treat sinus infections early
- Protect the face from trauma
- For patients using medications associated with duct narrowing, regular monitoring is advised
- Although not all cases can be prevented, good hygiene lowers the risk
Recovery and Prognosis – How Long Does Treatment Take?
Recovery varies depending on severity. Mild cases improve within days of starting antibiotics. Chronic cases may require weeks, especially if surgery is needed. After DCR, recovery takes 2-4 weeks.
Understanding dacryocystitis recovery time helps set expectations. Prompt intervention usually leads to complete recovery. Delayed care can result in complications such as orbital cellulitis or long-term tear duct damage.
When to See a Doctor
Seek medical attention immediately if you experience sudden swelling, redness, fever, vision changes or discharge. Babies with persistent tearing or sticky eyes should be evaluated promptly.
Conclusion – Effective Treatment Leads to Healthy Eyes
Dacryocystitis is manageable with timely care. Understanding the causes of dacryocystitis, recognising its symptoms, and following appropriate treatment steps lead to a fast and complete recovery.
While many acute cases resolve with antibiotics, chronic or recurrent infections may require dacryocystitis surgery. Early management, good hygiene and appropriate follow-up help protect eye health and prevent complications.