Cycloplegia refers to a temporary loss of the eye’s ability to focus on near objects. It occurs when the ciliary muscle, responsible for accommodation, becomes paralysed, affecting near vision and often causing pupil dilation.
This condition is common during eye examinations, certain treatments and some medical conditions. Understanding its causes and effects helps patients manage symptoms safely.
What Is Cycloplegia? Understanding the Condition
Many patients ask what cycloplegia is or seek a clear definition of cycloplegia. Medically, cycloplegia is defined as paralysis of the ciliary muscle, leading to impaired accommodation and difficulty focusing on close objects. This cycloplegia definition also includes associated pupil dilation, which makes the eyes more sensitive to light.
Cycloplegia is usually induced intentionally through medicated eye drops to relax the ciliary muscle. This helps eye specialists accurately measure refractive errors, especially in children, where focusing efforts can mask underlying issues.
How Cycloplegia Works
The ciliary muscle, iris and lens work together to adjust focus. In cycloplegia, anticholinergic medications block acetylcholine receptors in the ciliary body.
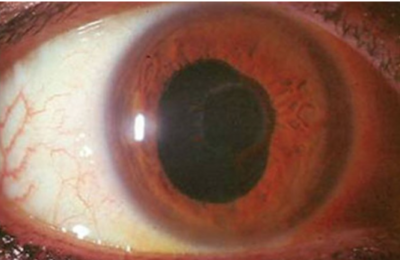
This results in paralysis of the ciliary muscle and enlarged pupils, also known as cycloplegia and mydriasis. The inability to adjust lens shape leads to blurred near vision.
Causes of Cycloplegia: Why It Happens
Most cases of cycloplegia are due to medicated eye drops used during diagnostic eye procedures. These drops temporarily paralyse the ciliary muscle to improve diagnostic accuracy. Other causes include neurological conditions, eye trauma, inflammation or tumours affecting the focusing mechanism.
H3: Medications That Cause Cycloplegia (Cycloplegic Agents)
Common cycloplegic drops include:
- Atropine: Lasts 7-12 days
- Cyclopentolate: Up to 24 hours
- Homatropine: 1-3 days
- Scopolamine: 3-7 days
- Tropicamide: 6-24 hours
Phenylephrine causes mydriasis without cycloplegia, creating dilation only. These medications have varying strengths and durations, and their use depends on clinical need.
H3: Other Factors and Conditions
Eye trauma, neurological disorders, and inflammation, such as uveitis, can also cause cycloplegia. Individuals with shallow anterior chambers may face increased risk due to pressure spikes when the pupil dilates.
Recognising the Symptoms of Cycloplegia
Typical cycloplegia symptoms include:
- Blurred near vision
- Difficulty reading or focusing up close
- Light sensitivity
- Headaches or eye strain
- Occasional dizziness
Distance vision usually remains unaffected. Most symptoms resolve once the eye drops wear off.
How Long Does Cycloplegia Last?
The duration depends on the medication used. Cyclopentolate may last only hours, while atropine can persist for days. Younger patients and those with lighter eye colours may experience longer recovery periods.
Cycloplegia vs Mydriasis and Presbyopia: Key Differences
|
Feature |
Cycloplegia |
Mydriasis |
Presbyopia |
|
Primary Effect |
Paralysis of the ciliary muscle. |
Simple dilation of the pupil. |
Age-related stiffening of the lens. |
|
Near Vision |
Loss of accommodation (inability to focus). |
Often unaffected (unless combined with cycloplegia). |
Permanent reduction in near focusing ability. |
|
Duration |
Temporary (usually drug-induced). |
Temporary. |
Permanent. |
|
Mechasims |
The ciliary muscle cannot contract to change lens shape. |
The iris opens the pupil wider. |
The lens becomes too rigid to change shape. |
Diagnosis of Cycloplegia: How Eye Specialists Assess It
Diagnosing cycloplegia often begins with assessing recent eye drop use. Specialists evaluate accommodation, light reactions, and conduct cycloplegic refraction, which is especially important in children to detect hidden farsightedness or accommodative spasm. Additional tests may be done if structural issues are suspected.
Treatment Options for Cycloplegia
Most cases resolve naturally as the medication wears off. Treatment for cycloplegia depends on the cause.
Managing Medication-Induced Cycloplegia
If cycloplegia is performed after an eye exam, no treatment is usually required. Vision returns gradually to normal. Patients may need temporary glasses for close work until accommodation returns.
Treating Underlying Conditions
For inflammation or infections, anti-inflammatory or antibiotic treatments may be prescribed. If neurological conditions are involved, medical management focuses on treating the underlying disease.
Therapeutic Use of Cycloplegic Agents for Pain Relief
Cycloplegic agents are also used intentionally for pain relief in conditions like uveitis and corneal abrasions. They stabilise the blood-aqueous barrier and prevent adhesions inside the eye, making them a key part of treatment in inflammatory eye diseases.
Vision Therapy and Assistive Devices
Short-term strategies such as corrective lenses, magnifiers or screen adjustments can help patients manage blurred near vision until recovery.
Side Effects and Risks of Cycloplegic Agents
Common cycloplegia side effects include burning, redness, blurred near vision and light sensitivity. Rare but serious systemic side effects may include confusion, fast heart rate or hallucinations. Patients with narrow angles are at risk of angle-closure glaucoma and should be assessed carefully before receiving strong dilating drops.
Self-Care and Recovery: Tips for Patients
Important recovery steps include:
- Wearing sunglasses to reduce glare
- Avoid driving until symptoms resolve
- Using adequate lighting for reading
- Taking breaks during close-up work
Preventing Cycloplegia: Safety Tips and Protective Measures
Preventing unnecessary cycloplegia involves supervised medication use, avoiding accidental contact with anticholinergic substances and protecting eyes from injury. Maintaining good hygiene and promptly treating eye conditions also reduces the risk.
Conclusion: Key Takeaways About Cycloplegia
Cycloplegia is a temporary condition that affects near vision by paralysing the ciliary muscles. Although commonly induced for clinical purposes, it can also result from trauma or disease.
With proper diagnosis, careful use of cycloplegic medications, and appropriate self-care, patients can expect full recovery. Those experiencing prolonged symptoms should seek advice from an eye specialist.









