What is Glaucoma?
Glaucoma is a silent thief of sight—one of the leading causes of irreversible blindness worldwide. This progressive eye disease damages the optic nerve due to increased intraocular pressure, leading to gradual vision loss. The most alarming part? It often creeps in without noticeable symptoms until significant damage is done.
Understanding glaucoma, its causes, symptoms, and prevention methods can help safeguard your vision.
What Are the Symptoms of Glaucoma?
Glaucoma is usually asymptomatic but may present with blurry vision, eye redness, and coloured haloes around lights. Blurry vision occurs when raised eye pressure causes corneal swelling and visual distortion. In most cases, vision loss develops gradually and may go unnoticed until advanced stages.
1. Loss of Vision
One of the most significant indicators of glaucoma is glaucoma vision deterioration, where blind spots appear in peripheral or central vision.
2. Blurry Vision
Blurred or hazy vision is an early warning sign, especially in angle-closure glaucoma where the pressure spikes suddenly.
3. Persistent Headache
High intraocular pressure can lead to intense headaches, often accompanied by eye pain.
4. Eye Redness
Redness in the eye is another symptom of glaucoma disease, indicating increased intraocular pressure or inflammation.
5. Stomach Upset, Nausea, and Vomiting
In acute cases, sudden pressure spikes can lead to nausea and vomiting, often misattributed to other conditions.
6. Pain in the Eye
Discomfort or severe pain in the eye may indicate phacolytic glaucoma or phacomorphic glaucoma, where lens changes obstruct normal fluid drainage.
7. Early Presbyopia
Difficulty focusing on nearby objects may suggest early onset of eye disorders linked to glaucoma.
Causes of Glaucoma
A blockage in the eye’s drainage system prevents proper outflow of aqueous fluid, leading to a rise in intraocular pressure. Sustained pressure damages the optic nerve fibres, gradually impairing vision and potentially causing irreversible vision loss.
1. Build-up of Aqueous Humor Inside the Eye
The eye maintains internal pressure by producing and draining aqueous humor. A blockage in this drainage system can lead to excessive pressure.
2. Genetic Reasons
Family history significantly increases the risk of developing glaucoma symptoms over time.
3. Birth Defects
Congenital defects in the eye’s drainage system can cause childhood glaucoma.
4. Blunt or Chemical Injury
Trauma or exposure to harmful chemicals can disrupt the normal flow of fluids inside the eye.
5. Acute Eye Infection
Certain infections cause inflammation and scarring, leading to glaucoma disease.
6. Blockage by Blood Vessels Inside the Eye
Poor circulation can cause vessel blockages, increasing the risk of glaucoma vision loss.
7. Inflammatory Conditions
Autoimmune diseases like uveitis can trigger secondary glaucoma.
Types of Glaucoma
Glaucoma is not a one-size-fits-all disease. It manifests in different forms, each requiring specific treatments.
Congenital Glaucoma
Present at birth due to improper development of the eye’s drainage system.
Lens Induced Glaucoma
Occurs when changes in the lens obstruct normal fluid drainage, leading to phacolytic glaucoma or phacomorphic glaucoma.
Malignant Glaucoma
A rare but severe form that can occur post-surgery, leading to rapid vision loss.
Secondary Glaucoma
Caused by medical conditions like diabetes, trauma, or prolonged use of steroids.
Pigmentary Glaucoma
What is Pigmentary Glaucoma? Pigmentary glaucoma is a type of secondary open angle glaucoma characterised...
Open Angle Glaucoma
The most common form, where pressure builds up gradually over time without early symptoms.
Closed Angle Glaucoma
A sudden increase in eye pressure due to blocked drainage, requiring immediate medical attention.
Phacomorphic Glaucoma
Phacomorphic Glaucoma: Causes, Symptoms, and Treatments Phacomorphic glaucoma is a severe eye disease that originates...
Acute Congestive Glaucoma
A sudden increase in eye pressure due to blocked drainage, requiring immediate medical attention.
Angle Recession Glaucoma
Rosette cataracts usually develop after an eye injury, creating a star-like pattern in the lens.
Pseudoexfoliation Glaucoma
Rosette cataracts usually develop after an eye injury, creating a star-like pattern in the lens.
Glaucoma Risk Factors
Are you at risk? Identifying these factors can help with early detection and prevention.
1. Are You Over 60 Years of Age?
Age is a significant risk factor, as the drainage system naturally weakens over time.
2. Have High Internal Eye Pressure?
Elevated intraocular pressure is a primary contributor to glaucoma.
3. Have a Family Member Diagnosed with Glaucoma?
A strong genetic link exists, making family history a key risk factor.
4. Have Certain Medical Conditions?
Diabetes, hypertension, and anemia increase glaucoma susceptibility.
5. Have Thin Corneas?
Thin corneas lead to inaccurate pressure readings, masking high intraocular pressure.
6. Have Extreme Nearsightedness or Farsightedness?
Severe refractive errors alter the eye’s anatomy, increasing glaucoma risk.
7. Have Had Eye Injuries or Surgeries?
Trauma and surgical procedures can alter fluid dynamics inside the eye.
8. Taking Corticosteroids for a Long Time?
Prolonged steroid use can trigger secondary glaucoma.
How to Prevent Glaucoma
While glaucoma cannot be completely prevented, early detection and lifestyle changes can slow its progression.
1. Have Eye Checkups Often
Routine eye exams allow for the early detection of glaucoma by monitoring intraocular pressure and optic nerve health. Identifying the condition early enables timely treatment, which can prevent or significantly slow down permanent vision loss.
2. Be Aware of Your Family’s Medical History
If glaucoma runs in your family, regular screenings are essential.
3. Keep Fit and Eat Healthy
A diet rich in leafy greens, omega-3 fatty acids, and antioxidants promotes eye health.
4. Protect Your Eyes While Performing Tasks That Could Cause Injuries
Wearing protective eyewear during sports or hazardous activities prevents trauma-induced glaucoma.
Glaucoma is a serious but manageable condition if diagnosed early. Prioritizing regular eye exams, understanding risk factors, and taking preventive measures can help protect your sight. If you experience any glaucoma symptoms, consult an eye specialist immediately.
Frequently Asked Questions (FAQs) about Glaucoma
Is glaucoma genetic?
Yes, glaucoma can be hereditary. A family history of the disease increases risk, making regular eye check-ups crucial for early detection and management, especially among close relatives.
What is the difference between ocular hypertension and glaucoma?
Ocular hypertension means raised eye pressure without optic nerve damage. Glaucoma involves both increased pressure and optic nerve damage, potentially causing vision loss if untreated. Regular monitoring differentiates them.
Can glaucoma occur in children?
Yes, though rare, glaucoma can develop in children. Known as congenital or juvenile glaucoma, it requires early diagnosis and treatment to prevent long-term vision impairment or blindness.
How often will I need follow-up appointments after glaucoma treatment?
Follow-up depends on disease severity and treatment type. Initially, visits may be frequent, later reducing to every few months for monitoring intraocular pressure and optic nerve health.
Can glaucoma affect both eyes?
Yes, glaucoma often affects both eyes, though severity may differ. One eye may develop symptoms earlier, but regular monitoring ensures both eyes are checked and treated appropriately.
Are there any natural remedies for glaucoma?
No proven natural remedies cure glaucoma. Healthy lifestyle habits may support eye health, but only medical treatments prescribed by an ophthalmologist effectively control eye pressure and protect vision.
Is glaucoma surgery painful?
No, glaucoma surgery is not painful. Local anaesthesia and sedation ensure comfort. Some patients may experience mild discomfort or irritation after the procedure, which usually subsides with recovery.
How should I prepare for glaucoma surgery?
Preparation includes following your doctor’s instructions, adjusting medications, arranging transport home, and discussing your health history. Fasting or avoiding certain drugs may be required before the procedure.
How long does glaucoma surgery take?
Glaucoma surgery typically takes 45 to 90 minutes, depending on the procedure type. Patients usually return home the same day, with recovery requiring follow-up visits for monitoring.
How common is glaucoma disease?
Glaucoma is a common eye disease that leads to the damage of the optic nerve. This damage to the optic nerve, which transmits information from the eyes to the brain, results in vision loss. If not treated properly, visual loss may be temporary or permanent. A change in the eye’s internal fluid pressure, also known as intraocular pressure (IOP), is the most common cause of Glaucoma.
Glaucoma affects around 70 million individuals globally. In 2020, glaucoma disease will affect over 80 million individuals worldwide, with the number anticipated to rise to over 111 million by 2040. Glaucoma is the main cause of irreversible blindness, accounting for 12.3% of all blindness worldwide.
What is the difference between an open angle and closed angle glaucoma?
Below we have given an insight into both these two types of glaucoma:
- Open angle glaucoma: The most prevalent type of glaucoma is open-angle glaucoma. It has no symptoms at first; however, side (peripheral) vision is lost at some time, and without treatment, a person can become completely blind.
- Closed angle glaucoma: Angle-closure glaucoma, also known as closed angle glaucoma, is a less prevalent kind of glaucoma. It happens when the drainage system in the eye gets fully obstructed, causing the pressure inside the eye to rapidly rise.
Can hereditary be one of the glaucoma causes?
Glaucoma can be inherited in some cases, and many experts around the world are researching genes and their effects on the disease. Glaucoma is not always hereditary, and the circumstances that lead to the beginning of the illness are yet to be fully understood.
What is considered as normal intraocular pressure?
The measurement of eye pressure is in millimetres of mercury (mm Hg). The typical range for eye pressure is 12-22 mm Hg, while pressures more than 22 mm Hg are considered abnormal. Glaucoma is not caused by high eye pressure alone. It is, nonetheless, a considerable risk factor. Individuals with high eye pressure should get comprehensive eye exams by an eye care specialist on a regular basis to screen for signs of glaucoma.
Is there a glaucoma cure?
Unfortunately, there is no glaucoma cure, and the vision loss resulted due to it is irreversible. If someone suffers from open-angle glaucoma, it has to be monitored for the rest of their life.
However, it is possible to slow down or stop additional vision loss using the medication, laser treatment, and surgery. The most important thing to remember here is that the first step in preserving your vision is to get a diagnosis. So, never ignore it if you experience any discomfort in your vision.
What's the difference between glaucoma and ocular hypertension?
When the classic optic nerve and vision alterations occur, glaucoma disease is diagnosed, usually with raised eye pressure but rarely with normal pressure. Ocular hypertension occurs when the intraocular pressure is higher than usual, but the person does not display indications of glaucoma.
What does 'tunnel vision' mean?
If not treated adequately in the early stages of glaucoma disease, it can severely affect the peripheral vision, leading to a condition known as ‘tunnel vision. Tunnel vision eliminates your ‘side vision,’ limiting your field of view to images in your central vision or straight ahead.
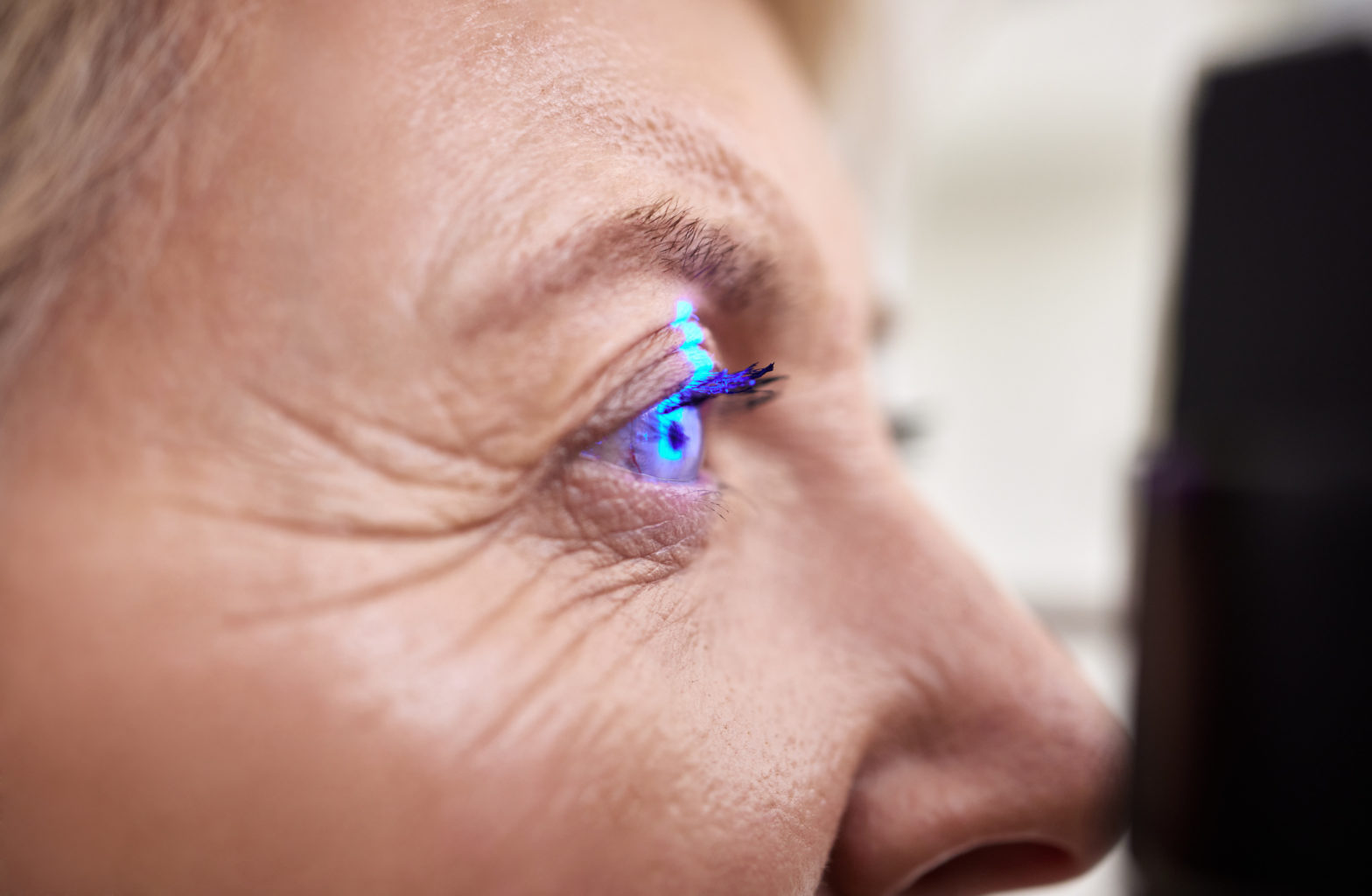
How does glaucoma disease get diagnosed?
If you feel that you are experiencing any glaucoma symptoms, it can be detected during a full dilated eye examination. The examination is straightforward and painless: your doctor will dilate (widen) your pupil with eye drops before checking your eyes for glaucoma and other eye issues.
A visual field test is included in the exam to examine your side vision. People with a family history of glaucoma should have their eye pressure and optic nerves tested frequently since they are at a higher risk of developing the condition.
This information is for general awareness only and cannot be construed as medical advice. Recovery Timelines, specialist availability, and treatment prices may vary. Please consult our specialists or visit your nearest branch for more details.Insurance coverage and associated costs may vary depending on the treatment and the specific inclusions under your policy. Please visit the insurance desk at your nearest branch for detailed information.
Do not ignore eye trouble!
Now you can reach our senior doctors by booking an online video consultation or a hospital appointment
Book an appointment now